In healthcare, small billing mistakes can lead to lost revenue, denied claims, and patient dissatisfaction. Aveta’s AI-powered RCM solution is built to fix that.
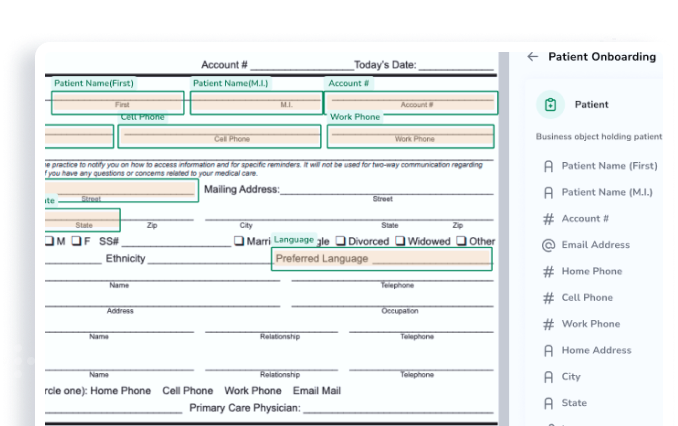
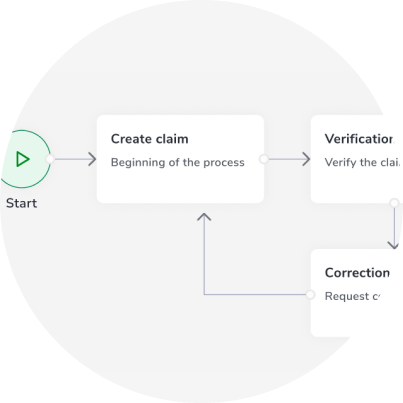
Our intelligent AI agents handle the entire revenue cycle—from smooth patient onboarding to fast, accurate claims submission—so your team can focus on care, not paperwork. Reduce denials, improve reimbursements, and streamline payment collection with ease.
Stay in control with real-time dashboards and detailed management reports that keep you informed every step of the way. Aveta also integrates with major insurance providers, including Medicare, to automate eligibility checks, prior authorizations, and electronic claims for inpatient and outpatient services.